Learn the EIP to EPL Tendon Transfer surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the EIP to EPL Tendon Transfer surgical procedure.
The extensor pollicis longus (EPL) tendon extends the thumb interphalangeal joint and also contributes to metacarpophalangeal joint extension. It serves an important role in hand opening and fine control of thumb position.
Although an acute injury resulting in division of the tendon will merit direct repair, many other causes of EPL dysfunction may be treated by tendon transfer. The commonest indication for EIP to EPL transfer is following attrition rupture of the EPL in the 3rd extensor compartment of the wrist associated with a distal radius fracture.
The commonest and certainly the simplest donor tendon to transfer to EPL is the extensor indicis proprius tendon in such cases.

INDICATIONS:
The patient in this case had a spontaneous rupture of the EPL tendon following a distal radius fracture that was treated non-operatively in a plaster cast. This is a common mechanism of injury and is thought to result from attrition rupture of the tendon secondary to extravasation of blood and possibly fracture debris into a tight third extensor compartment. A watershed zone within the intrinsic blood supply to the EPL tendon is also thought to be a contributing factor.
Other causes of a closed rupture may include inflammatory arthropathy such as rheumatoid arthritis or other forms of synovitis or tenosynovitis. Such ruptures have also been attributed to steroid therapy, excessive abnormal wrist motion, or a bony spur at the distal radius or scaphoid.
An open laceration of EPL may also require EIP to EPL tendon transfer if for example, presentation is delayed and primary repair is not possible or in cases where primary repair has failed.
It is important to note that a lack of EPL function as part of a non-recovering radial nerve palsy will usually also result in EDC and EIP dysfunction. Various alternative surgical options are described elsewhere for radial nerve palsy.
SYMPTOMS & ASSESSMENT:
The patient will usually present with weakness in thumb MCP extension and a lack of IPJ extension.
This may be accompanied by acute pain, particularly at the time of rupture and is typically felt over Listers tubercle. Pain is often not a predominant feature in spontaneous rupture at the time of presentation.
The clinical examination must include a test to establish the presence of EDC and EIP to the index finger
INVESTIGATION:
In cases where the diagnosis is in doubt, imaging using ultrasound may be useful. This can also help establish discontinuity in EPL as well as presence of the donor tendon. It may also demonstrate synovitis or tenosynovitis.
X-ray can be used to demonstrate the presence of a bony spur or other degenerative change.
OPERATIVE ALTERNATIVES:
As mentioned above, direct repair or interposition graft may be suitable options in select cases. Equally, some patients may be better served by an arthrodesis.
NON-OPERATIVE ALTERNATIVES
In patients that are not suitable for any form of surgery, functional outcome is likely to be poor. In very low demand patients one may consider non-operative management. Often an occupational therapist may be able to assist with a custom made splint.
CONTRAINDICATIONS:
Caution is advised operating on those patients with poor skin quality or poor vascularity. Poor pre-existing thumb function, for example secondary to advanced arthritic disease of the IPJ may mean that a tendon transfer does not have the desired effect. It is, as ever important to assess each patient as an individual and discuss the risks and benefits of surgery with him/her.

The patient is appropriately anaesthetised using either general anaesthesia or a regional anaesthetic block technique.
The patient is positioned supine with the limb positioned on an arm table. An upper arm tourniquet is used and inflated prior to commencing the procedure.
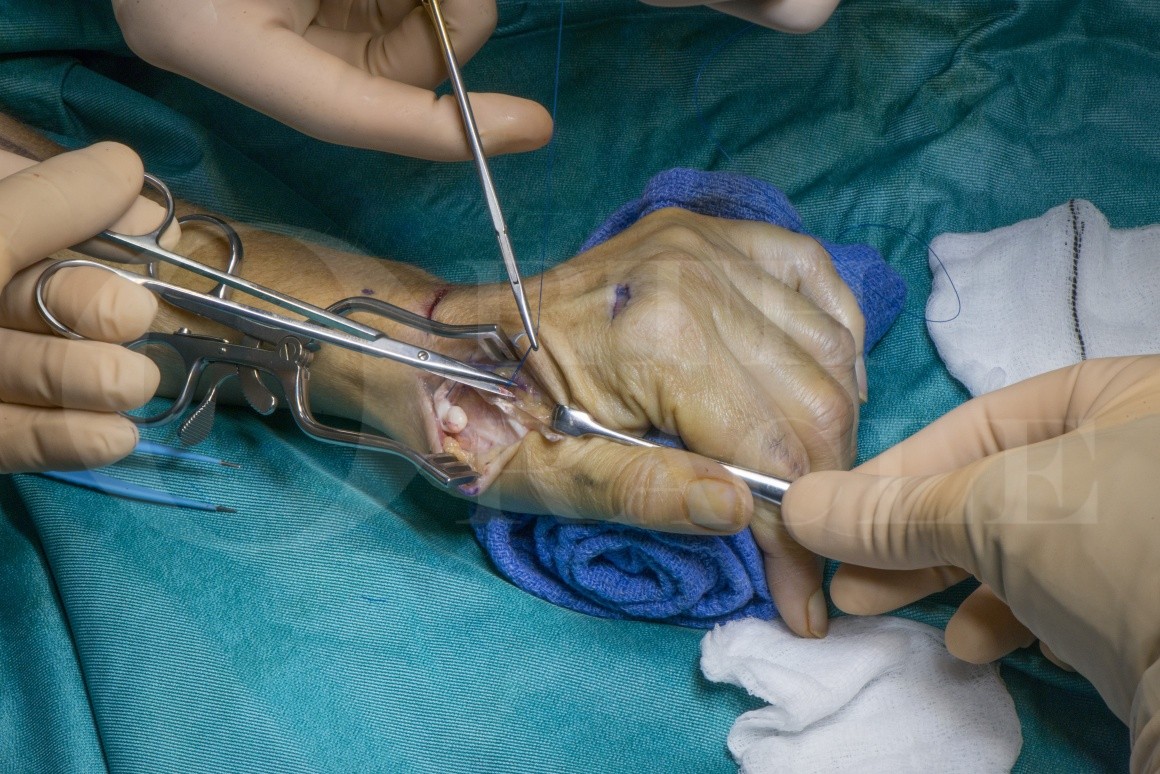
Three incisions are marked out. A 1cm transverse incision over the index MCPJ, a 1-2cm transverse incision overlying the EIP just distal to the extensor retinaculum, and finally a 2-3 cm longitudinal incision over the EPL tendon at the thumb metacarpal.
Tendon instruments and bipolar diathermy are required.

The patients wounds are reviewed at 1 week and a splint can be fashioned at this stage to hold the thumb in extension and abduction with the wrist extended at 30 degrees.
At 4 weeks the patient should commence gentle thumb mobilisation exercises with intermittent splintage, and at 6 weeks the splint may be discarded.
A good hand therapist is essential to guide and tweak this rehabilitation process as appropriate for individual patients.

Excellent results have been widely reported. In 1997 De Smet followed up 13 patients and found good or excellent results in 12. There was often an extension lag at the thumb IPJ and MCPJ. Dexterity and grip force were excellent. Extension force at the index finger was reduced to 65% of the contralateral side.
Acta Orthop Belg. 1997 Sep;63(3):178-81.
The procedure is more reliable at restoring thumb extension than tendon grafting, direct repair or other types of tendon transfer.
Hand Clin. 1995 Aug;11(3):411-22
Biomechanical studies show that the moment arm and mechanical properties of the EIP transfer via a subcutaneous tunnel closely resemble that of the EPL.
J Hand Surg Am. 2003 Jul;28(4):661-8
Jan Friden and colleagues have used a cadaveric model to demonstrate stronger and stiffer tendon coaptation using a single tendon pass with a side to side suture technique, when compared to the traditional Pulvertaft weave. This may allow earlier loading with fewer adhesions.
J Hand Surg Am. 2010 Apr; 35(4): 540–545.
Reference
- orthoracle.com


























